Rotator Cuff Arthropathy
The term “cuff tear arthropathy” was first reported in 1983 by Dr. Charles Neer(1), the head of the esteemed Columbia Shoulder Service (New York City) and considered by many to be the father of modern shoulder surgery. Dr. Neer would go on to train and mentor shoulder surgeon Dr. Obermeyer’s mentor, Dr. Evan Flatow at Columbia. Dr. Neer described cuff tear arthropathy as a condition characterized by rotator cuff insufficiency, degenerative arthritis of the shoulder (glenohumeral) joint, swelling, and erosion of the skeletal architecture of the shoulder. This condition was commonly seen in older patients who were thought to have chronic and untreated rotator cuff tears that have progressed to the extent that the joint of the shoulder becomes involved and progressively eroded.
Anatomy and Biomechanics of Rotator Cuff Arthropathy
The rotator cuff is an anatomic term that refers to the coalescence of the tendons of four muscles, the supraspinatus, the infraspinatus, the subscapularis, and the teres minor. This “cuff” provides a critical stabilizing role in capturing and holding the humeral head (ball) in the glenoid socket of the shoulder. The compressive forces generated allow the ball to stay in the shallow dish of the glenoid socket while the bigger powerful deltoid muscle lifts the arm through a range of motion. This is different than other ball-and-socket joints, such as the hip, where the bony constraint of a full cup allows the ball to remain in place. When the rotator cuff tears, the deltoid forces continue to pull on the humeral head and the tear progresses, leading to shifting of the head up and out of the socket. Dr. Neer’s initial description of this phenomenon is still observed today; leading to trauma and erosion of the joint surface of the shoulder, in part due to pain and disuse osteopenia coupled with the abnormal forces pulling the rounded humeral head out of the concave glenoid socket. The result of this chronic process is characteristic radiographic changes where the shoulder takes on features of the hip, including rounding of the acromion roof bone where is appears similar to a hip socket “acetabularization” and the humeral ball losing the contour of the bump (tuberosity) of the humerus bone “femoralization”.
Diagnosis of Cuff Arthropathy
While the condition is more common in women, it also affects men. Swelling, pain (day and night), and loss of function are typical. The average duration of pain symptoms is several years, averaging 9.8 years in Neer’s initial description(1). Clinical findings typically include swelling of the shoulder, atrophy of the rotator cuff muscles, and weakness suggestive of a massive rotator cuff tear. Most patients cannot lift the arm overhead, a condition known as pseudoparalysis, and also have substantial difficulty or inability to position the arm away from the body (loss of external rotation). Crepitus, which is a crunching sensation of the bones with motion, is also seen. The diagnosis is confirmed on imaging were the humeral head is sitting superiorly out of the glenoid socket, rounding of the upper humerus (femoralization), and indentation/erosion of the acromion process (acetabularization). These findings are in contradistinction to those seen in primary shoulder arthritis, where there are spurs (osteophytes) seen on the lower (inferior) head and posterior wear of the glenoid socket.
Treatment of Cuff Arthropathy
The initial treatment of cuff arthropathy is nonsurgical. Modification of activities, gentle use, and sometimes corticosteroid injections are temporarily helpful. Depending on the status of the glenohumeral joint, sometimes a structured exercise program is recommended, which can be initiated under the direction of physical therapy. The objective of therapy for this condition is to strengthen and optimize the remaining rotator cuff muscle, re-educate the shoulder blade muscles to compensate for the shoulder damage.
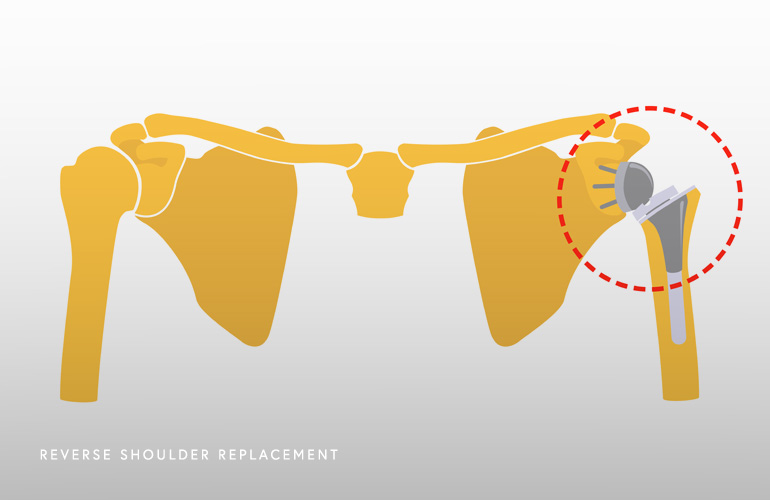
In patients that are healthy enough for surgery and willing to undergo a period of rehabilitation, the standard of care for rotator cuff arthropathy is reverse shoulder replacement. The reverse shoulder replacement achieves both pain relief and functional restoration by capturing and holding the humerus bone in the socket as a result of flipping the geometry/concavity of the shoulder. In this procedure, a metal ball is fixated to the glenoid socket and a partial cup is fixated into the humerus bone. This technology was initially developed in France by a surgeon named Paul Grammont in the 1980s(2) as a way of using a prosthesis to fix the fulcrum of the shoulder so that the powerful deltoid muscle could lift and power the arm for motion. This prosthesis works by lengthening the humerus and moving the shoulder’s center of rotation towards the native glenoid bone, so that the deltoid muscle is efficient and able to effectively bypass the torn and deficient rotator cuff.
Since the reverse shoulder replacement had achieved widespread adoption in the United States in the early 2000s, it has revolutionized the field of shoulder surgery. The prosthesis design continues to be refined and improved and the complication rate is very low with overall excellent clinical outcomes. Shoulder surgeon Dr. Obermeyer performs reverse shoulder replacement as a large part of his clinical practice, and if you have been struggling with pain and difficulty with use of the shoulder for some time, Dr. Obermeyer will review your diagnosis and discuss whether reverse shoulder replacement is right for you.
- Neer CS 2nd, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am. 1983 Dec;65(9):1232-44. PMID: 6654936.
- Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005 Jan-Feb;14(1 Suppl S):147S-161S. doi: 10.1016/j.jse.2004.10.006. PMID: 15726075.
At a Glance
Dr. Thomas Obermeyer
- 15+ years of training and experience treating complex shoulder and sports medicine conditions
- Expert subspecialized and board-certified orthopedic care
- Award-winning outstanding patient satisfaction scores
- Learn more

