Calcific Tendonitis
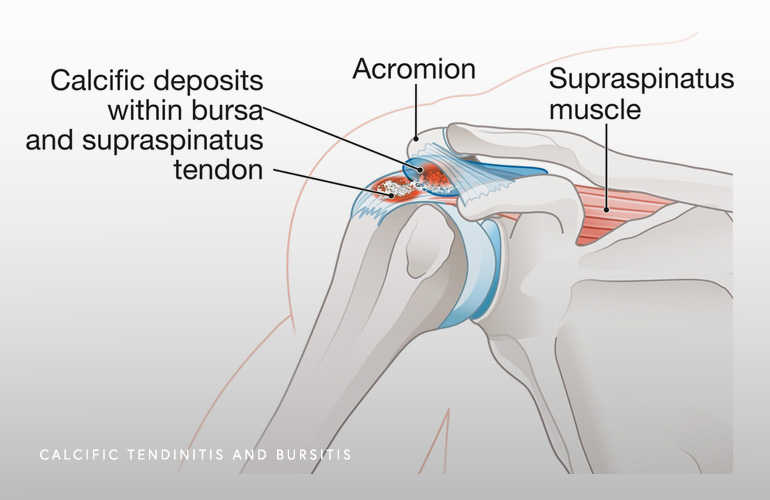
Calcific tendonitis is a painful condition of the shoulder of where calcium crystals start to form within the rotator cuff tendon(1). Why the rotator cuff is such a frequent location of this crystal formation is unknown. The generation of pain from calcific tendonitis results from these calcium crystals pushing on and irritating the surrounding rotator cuff tendon and bursal tissue, which is a highly sensitive area of the shoulder. There is some new research suggesting that the crystals stimulate an inflammatory response, and that some of the pain is mediated by the formation of new blood vessels and nerves that develop in the tendon tissue affected by the crystal formation(2).
The causes of calcific tendonitis are unknown, a condition in medicine known as “idiopathic”. Most of the time, the condition just happens, and there no clear event or causative injury. Other times, there is a subtle amount of calcium developing in the rotator cuff tendon, that the patient may not even realize, and then there is an injury or event that sets off the body’s inflammatory healing response, which can cause pain.
There are no clear associations between problems with systemic calcium homeostasis, and just because you are diagnosed with calcific tendonitis does not mean you have high calcium or a problem with the way your body manages calcium levels. Research on this is ongoing. What we do know is that when you are diagnosed with calcific tendonitis, you are more likely to develop the same problem on the other shoulder, which may support the hypothesis there is a genetic predisposition. There is no clear link between activities or status of the rotator cuff tendon, as younger adults are more often affect by the disease, and the process is well known to occur in an otherwise healthy rotator cuff tendon.
Sometimes the pain from calcific tendonitis occurs over a short period, and the condition is called acute calcific tendonitis, where the rotator cuff becomes extremely painful, and it is likely that the deposited calcium start to leak into the sensitive area called the subacromial bursa. Pain is typically experienced at the front and lateral shoulder, radiating to the upper arm, and movements are so painful that is frequently more comfortable to hold the arm in a protective position near the body. In more chronic cases of calcific tendonitis, the symptoms can parallel those of a more generic rotator cuff disorder, with pain, difficulty with use, problems laying on the affected side occurring, among others.
The gold standard for diagnosis of a calcific deposit in the shoulder is a series of standard radiographs (X-rays). The X-rays are taken in different planes to help identify the size, location, and texture of the deposit. Ususally the diagnosis is very clear on the front-to-back projection, although careful evaluation of all views are necessary to observe a deposit that is obscured by the overlying humeral head. The standard radiographic series can be useful to not only diagnose but also follow the progression of the diseae. Sometimes MRI can be used to confirm in three dimensions the appearance of the deposit, to identify any other abnormalities in the shoulder, and to help plan for arthroscopic (surgical) removal, when necessary.
The treatment of calcific tendonitis can consist of a trial of oral medications, a corticosteroid injection, and physical therapy. Often when the condition is highly painful, or has been occurring over weeks to months, shoulder surgeon Dr. Obermeyer may discuss with you a procedure performed in the office under local anesthesia called barbotage, which involves identifying the deposit and repeatedly inserting and removing a needle while a corticosteroid is administered, delivering a two-fold therapeutic benefit. First, the barbotage involves a mechanical disruption of the deposit, which not only immediately allows dissipation in the calcium crystals present but allows the healing cells of the body access to remove the remainder of any calcium on their own. Secondly, the corticosteroid injection part of the barbotage permits the administration of a cortisone medication right into the area of abnormality, which improves pain and allows patients to resume activities.
There is a small fraction of patients diagnosed with calcific tendonitis (~10%) that do not respond to some of the treatments mentioned above and require arthroscopic removal. This is performed as an outpatient procedure which allows Dr. Obermeyer to see the deposit and remove it with arthroscopic instruments. This is done minimally invasively as an outpatient, and allows Dr. Obermeyer to treat any concurrent pathology in the shoulder. If there is a large amount of calcium in the tendon, sometimes after the calcium is removed the surrounding rotator cuff tissue requires a small repair. Dr. Obermeyer will discuss with you the specifics of your individual case so you know what to expect at the time of the procedure based on your individual circumstances. Generally, the outcomes of arthroscopy for this condition are excellent with complete eradication of the problem in the majority of cases on final follow up.
Schedule an orthopedic appointment
If you have pain in your shoulder and are concerned you may require an orthopedic subspecialist evaluation, call our office, or book an appointment with shoulder surgeon Dr. Thomas Obermeyer. Dr. Obermeyer provides expert orthopedic care for patients suffering Calcific Tendonitis. Dr. Obermeyer has orthopedic offices in Schaumburg, Bartlett, and Elk Grove Village, Illinois. Dr. Obermeyer regularly sees patients from throughout Illinois including Hoffman Estates, Palatine, Elgin, Streamwood, Arlington Heights, and Roselle communities.
References
- Uhthoff HK, Loehr JW. Calcific Tendinopathy of the Rotator Cuff: Pathogenesis, Diagnosis, and Management. J Am Acad Orthop Surg. 1997 Jul;5(4):183-191. doi: 10.5435/00124635-199707000-00001. PMID: 10797220.
- Hackett L, Millar NL, Lam P, Murrell GA. Are the Symptoms of Calcific Tendinitis Due to Neoinnervation and/or Neovascularization? J Bone Joint Surg Am. 2016 Feb 3;98(3):186-92. doi: 10.2106/JBJS.O.00417. PMID: 26842408.
At a Glance
Dr. Thomas Obermeyer
- 15+ years of training and experience treating complex shoulder and sports medicine conditions
- Expert subspecialized and board-certified orthopedic care
- Award-winning outstanding patient satisfaction scores
- Learn more

