Multidirectional Instability
What is Multidirectional Instability?
Multidirectional instability (“MDI”) is defined as the presence of pain or symptoms from soft tissue imbalance that leads to the shoulder joint sliding (translating) in position in two or more directions. Usually this condition is seen in young patients in the second or third decade of life, many of whom have abnormal laxity of the joints, where a combination of predisposing factors such as young age and pliable tissue coupled with repetitive activity demands (such as volleyball, swimming, or gymnastics) lead to repetitive microtrauma and therefore pain. Although having MDI can become symptomatic and cause problems for athletic performance during in-season competition, it can also affect patients outside of sporting season and occur in patients without any particular recreational or athletic pursuits.
MDI is unique from other forms of instability of the shoulder as there frequently is an absence of a single traumatic event reported, the symptoms develop gradually and insidiously, and sometimes can be observed on both shoulders. The observation that MDI can affect both shoulder supports the theory that there may be a congenital (inborn) predisposition to developing this condition(1). Unlike traumatic instability where there is clear structural damage to the shoulder that frequently requires surgical repair, MDI has more subtle anatomic abnormalities that are often not immediately evident on advanced imaging, and is less commonly managed with surgical treatment.
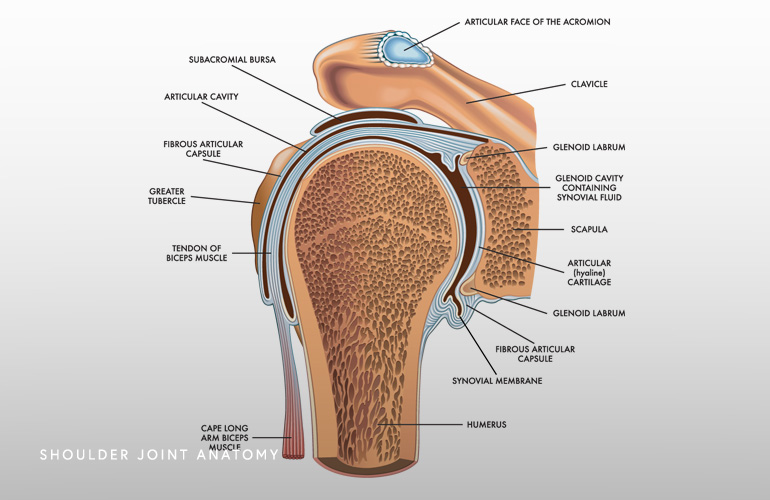
The shoulder (glenohumeral) joint has limited inherent bony stability due to the relatively flat and minimally concave glenoid socket that leave it relatively loose without well functioning surrounding soft tissues that hold it in position. The labrum, which is a bumper of cartilage that deepens the socket only minimally, helps to an extent, and the remaining stability is largely dependent on the ligaments which connect the ball to the socket and are effectively the checkrein that get tight at the limits of motion and keep the ball in socket. These ligaments are characteristically loose in MDI and it has also been observed that the socket in MDI patients is also shallower than age-matched controls(2). This looseness of the tissues is often all that is observed on MRI scans of patients developing MDI (called “patulousness”), and although there can be a coexistence of labral tears and cartilage abnormalities, frequently clear tearing is not seen. Ultimately it is the looseness of the tissues coupled with the shallowness of the socket that lead to abnormal sliding or translation of the humeral ball which leads to tissue irritation and pain.
Compounding the pathologic laxity seen in MDI is the frequently observed dysfunction in the muscles surrounding the shoulder girdle. When the shoulder becomes unstable, there may be adaptive involuntary changes in the activation of the shoulder blade musculature, a condition called dyskinesia. This can further lead to pain from the fatigue and strain on the shoulder blade muscles.
The primary symptom in multidirectional instability is pain which is deep in the shoulder and sometimes variable in the way that it is explained by patients. The pain is typically poorly localized and is observed in the shoulder blade and often down the arm. Some patients may report numbness and tingling which is worse with activity. Athletes may experience a deterioration of athletic performance, particularly those athletes with high demand overhead activities. The physical examination of the shoulder is critical in the diagnosis of MDI, as there are findings suggesting laxity of the tissues of the shoulder and of other joints, and of abnormal shifting of the shoulder in multiple directions.
The primary treatment of multidirectional instability is rehabilitative strengthening of the rotator cuff and scapular muscles. The rotator cuff functions as a wrapping tissue onto the ball of the shoulder that pulls and compresses it into the socket; strengthening the rotator cuff muscles can improve the symptoms of MDI. Referral to physical therapy can identify and correct dyskinesia of the shoulder blade muscles, which improves the function of the shoulder over time, and ultimately improves pain. Overhead athletes may require a period of activity modification and refrain from sport while the rehabilitative process is initiated. Ultimately participating in sports despite pain can lead to exacerbation and prolongation of symptoms.
For patients in whom physical therapy, modification of activities, and home exercises have been unsatisfactory, advanced arthroscopic techniques are now available to decrease ligament laxity, tighten the shoulder, and correct symptoms in a minimally invasive manner. The historical operation for MDI was an open “capsular shift”(3) which involved detachment of one of the rotator cuff tendons for exposure and then tightening the ligaments in an open fashion. It is now believed that advanced arthroscopic techniques can achieve the same degree of ligament tightening “plication” as open surgery, with improvements in the precision of where the tensioning occurs in the shoulder, better arthroscopic diagnosis of pathology, lessened surgical morbidity, and more favorable outcomes. Innovations in arthroscopic implants allow tensioning “plication” of the ligaments in a low-profile, well tolerated manner without the requirement for knots and irritating material retained in the shoulder joint.
Schedule an orthopedic appointment
Are you or a loved one suffering from a multidirectional shoulder instability? Call or make an appointment online with shoulder surgeon Dr. Thomas Obermeyer. Dr. Obermeyer is widely regarded as one of the best shoulder surgeons in Illinois. Dr. Obermeyer has orthopedic offices in Schaumburg, Bartlett, and Elk Grove Village, Illinois. Dr. Obermeyer regularly sees patients from throughout Illinois including Hoffman Estates, Palatine, Elgin, Streamwood, Arlington Heights, and Roselle communities.
- Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res. 2002 Jul;(400):65-76. doi: 10.1097/00003086-200207000-00009. PMID: 12072747.
- von Eisenhart-Rothe R, Mayr HO, Hinterwimmer S, Graichen H. Simultaneous 3D assessment of glenohumeral shape, humeral head centering, and scapular positioning in atraumatic shoulder instability: a magnetic resonance-based in vivo analysis. Am J Sports Med. 2010 Feb;38(2):375-82. doi: 10.1177/0363546509347105. Epub 2009 Nov 25. PMID: 19940294.
- Neer CS 2nd, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am. 1980 Sep;62(6):897-908. PMID: 7430177.
At a Glance
Dr. Thomas Obermeyer
- 15+ years of training and experience treating complex shoulder and sports medicine conditions
- Expert subspecialized and board-certified orthopedic care
- Award-winning outstanding patient satisfaction scores
- Learn more

