Knee Osteoarthritis
Anatomy
The knee is the largest and strongest joint in the body, sustaining large loads to support weightbearing and ambulation. The knee joint can be separated into three distinct “compartments” which each have unique patterns of disease, the medial (inside), the lateral (outside), and patellofemoral (front). One feature the three compartments share is the presence of smooth, slippery lining called articular cartilage that protects and cushions the bones when the knee moves. The medial and lateral compartments additionally have tissue called the meniscus which functions to stabilize the bones and serve as a shock absorber, dissipating some of the forces the cartilage sustains. The knee joint is also surrounded by a lining called the synovium which is like a sheath that provides fluid to lubricate the moving surfaces and reduce friction.
Osteoarthritis is the most common form of arthritis in the knee and is commonly known as “wear-and-tear” arthritis. The “-itis” part of osteoarthritis indicates an inflammatory process of the joint, which is where the body’s enzymes and cell signaling chemicals contribute to the breakdown of the cartilage lining of the knee. It is also this inflammation that causes pain. While it is true that mechanical factors such as high chronic loads to the joint can contribute to breakdown of the tissues, the factor that accelerates destruction of the cartilage is the process of inflammation.
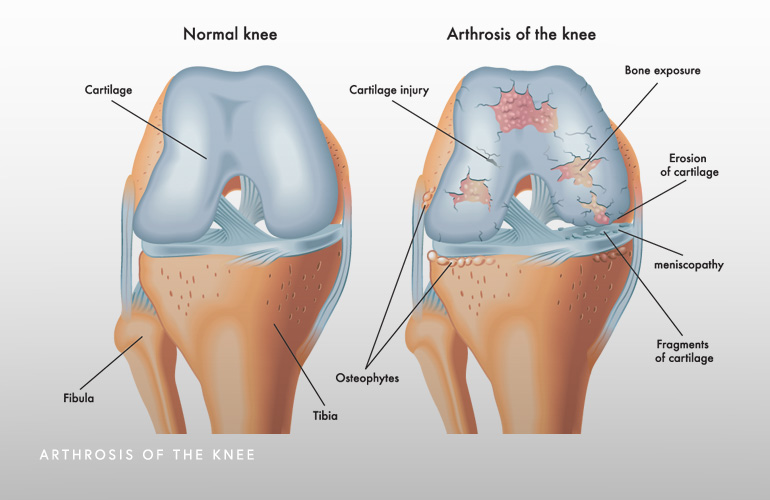
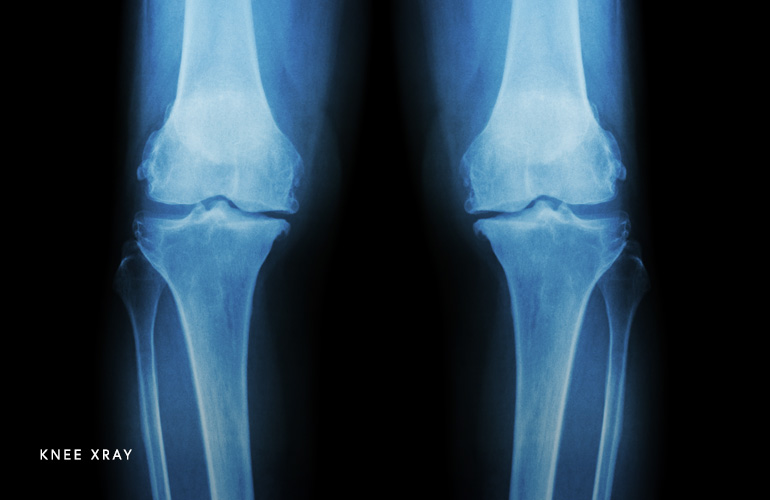
Osteoarthritis is diagnosed based on a combination of clinical factors such as pain, examination of the knee, and imaging findings. As the osteoarthritis advances, radiographs (X-rays) have characteristic findings. Some of these findings including loss of the joint space (the gap between the bones narrows), sclerosis (hardening of the bone from the lost padding), cysts (tiny cavities where in the bone where little holes form), and osteophytes (spurs). In milder cases, an MRI is needed to see the process because it has not advanced to the point that X-rays look different. On MRI, the cartilage lining has thinned and bone edema is evident (fluid reaction under the joint where the cartilage has been lost). The most sensitive way of knowing if osteoarthritis is present in the knee is on arthroscopy, where a camera can physically inspect the cartilage lining of the knee. Using live videography, the cartilage is observed and evidence of fraying, cracks, or loss of the cartilage suggests the presence of osteoarthritis.
Pain in the knee is the cardinal symptom of osteoarthritis. As the disease progresses, pain may be present at night, at rest, and with progressively more simple activities such as walking, getting up the stairs, and sitting for prolonged periods. Sometimes the knee will feel as though it is buckling or giving out. When the knee is examined, findings such as tenderness to touch, loss of motion, swelling, deformity (crookedness of the joint) are present.
Treatment for osteoarthritis depends on the severity of the pain, the chronicity of symptoms, and the degree of functional impairment. For mild forms of osteoarthritis, initial therapy includes modification of activity, and initiation of low-impact aerobic exercise such as walking, cycling, rowing, and swimming or deep water running. Many patients in this category will benefit from physical therapy, where specific range of motion and strengthening exercises are started and supervised by a licensed physical therapist. Anti-inflammatory medications such as ibuprofen, naproxen, or meloxicam can be helpful. Sometimes anti-inflammatory creams applied locally to the knee can be worth trying, as well as heat and ice. Almost universally, weight loss can be helpful for improving symptoms from osteoarthritis, in large part because losing weight can lessen the load or force through the joint. Several studies have shown a dose-response relationship between weight loss and improvement in symptoms(1). Nutritional supplements and glucosamine/chondroitin have limited demonstrated effectiveness(2).
Injections such as corticosteroids can be effective for many patients with knee osteoarthritis who have more severe symptoms that have either not responded to other treatments, have only experienced pain for a short period of time or are looking for short-term relief, or who are not candidates for surgery. Typically, the steroid medication methylprednisolone is used, which is a powerful anti-inflammatory that works directly in the diseased knee joint. The anti-inflammatory properties of the steroid help curb the pain, which sometimes lasts for a month or two in favorable circumstances. Sometimes the relief is only very short-lived, however, and the duration of relief is often difficult to predict. Often, patients with milder forms of arthritis with more severe pain symptoms and swelling can respond well(3). There is a mild degree of toxicity to the remaining cartilage in the setting of knee osteoarthritis, so patients that are younger with milder forms of arthritis might consider using corticosteroid injections judiciously.
Bracing can be helpful for certain patients where the arthritic disease process preferentially affects one side of the knee (most commonly the inner or medial part) and the arthritic disease affects the alignment of the leg. The alignment is quantified on radiographs and physical examination and can be assessed by knee surgeon Dr. Obermeyer. The purpose of bracing in knee osteoarthritis is to “open up” or “unload” the worn and damaged inner section of the knee so the load is transferred to the other parts of the knee. This so-called unloader bracing is done in select patients, and because the braces are sometimes hot and uncomfortable, can be best used for selected portions of the day (for example at work) when long periods of standing are necessary and when the brace can be custom-fitted to the patient’s leg. These unloader braces, when tolerated, have shown to be slightly more effective than simple neoprene sleeve or other types of over-the-counter braces(4).
Surgery in the form of total knee replacement is considered the gold standard for knee osteoarthritis. Knee replacement consists of resection of the disease articular (joint) surfaces of the knee and replacement with resurfacing with metal and polyethylene prosthetic components. In patients that are candidates for knee replacement, the procedure can provide significant pain relief as well as improved function and quality of life. Due to the popularity, favorable outcomes, and improved access, the annual number of total knee replacements in the United States is expected to increase to approximately one million procedures by the year 2030(5).

Schedule an orthopedic appointment
If you have knee pain and are concerned you may require an orthopedic subspecialist evaluation, call our office, or book an appointment with knee surgeon Dr. Thomas Obermeyer. Dr. Obermeyer provides expert orthopedic care for patients suffering knee osteoarthritis. Dr. Obermeyer has orthopedic offices in Schaumburg, Bartlett, and Elk Grove Village, Illinois. Dr. Obermeyer regularly sees patients from throughout Illinois including Hoffman Estates, Palatine, Elgin, Streamwood, Arlington Heights, and Roselle communities.
References
- Riddle DL, Stratford PW. Body weight changes and corresponding changes in pain and function in persons with symptomatic knee osteoarthritis: a cohort study. Arthritis Care Res (Hoboken). 2013 Jan;65(1):15-22. doi: 10.1002/acr.21692. PMID: 22505346; PMCID: PMC3401342.
- Roman-Blas JA, Castañeda S, Sánchez-Pernaute O, Largo R, Herrero-Beaumont G; CS/GS Combined Therapy Study Group. Combined Treatment With Chondroitin Sulfate and Glucosamine Sulfate Shows No Superiority Over Placebo for Reduction of Joint Pain and Functional Impairment in Patients With Knee Osteoarthritis: A Six-Month Multicenter, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Arthritis Rheumatol. 2017 Jan;69(1):77-85. doi: 10.1002/art.39819. Erratum in: Arthritis Rheumatol. 2017 Oct;69(10 ):2080. PMID: 27477804.
- Maricar N, Callaghan MJ, Felson DT, O’Neill TW. Predictors of response to intra-articular steroid injections in knee osteoarthritis–a systematic review. Rheumatology (Oxford). 2013 Jun;52(6):1022-32. doi: 10.1093/rheumatology/kes368. Epub 2012 Dec 22. PMID: 23264554; PMCID: PMC3651612.
- Moyer RF, Birmingham TB, Bryant DM, Giffin JR, Marriott KA, Leitch KM. Valgus bracing for knee osteoarthritis: a meta-analysis of randomized trials. Arthritis Care Res (Hoboken). 2015 Apr;67(4):493-501. doi: 10.1002/acr.22472. PMID: 25201520.
- Sloan M, Premkumar A, Sheth NP. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018 Sep 5;100(17):1455-1460. doi: 10.2106/JBJS.17.01617. PMID: 30180053.
At a Glance
Dr. Thomas Obermeyer
- 15+ years of training and experience treating complex shoulder and sports medicine conditions
- Expert subspecialized and board-certified orthopedic care
- Award-winning outstanding patient satisfaction scores
- Learn more

