Is Your Back Causing Shoulder Pain?
A Patient’s Guide to Differentiating Intrinsic Shoulder Problems from Cervical Nerve Problems (Referred Pain)
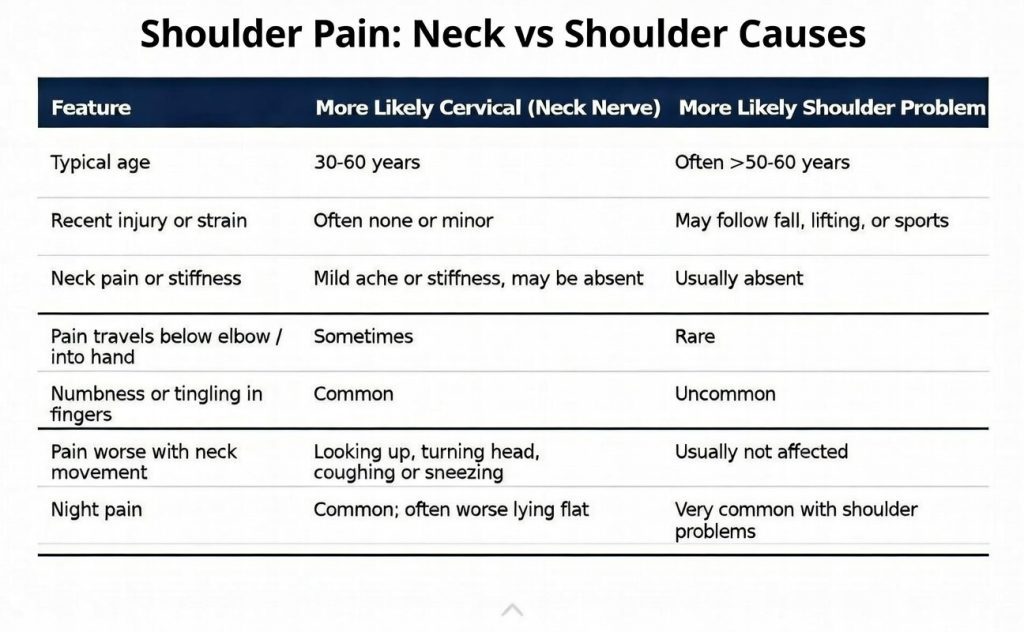
Shoulder pain is a very common problem and while many assume the problem must be in the shoulder — rotator cuff tear, impingement, arthritis, frozen shoulder, or labral injury — a significant percentage of “shoulder pain” actually originates from the cervical spine (the neck). This is called cervical radiculopathy or referred pain from the neck, and missing it is one of the main reasons patients fail conservative treatment or undergo unnecessary shoulder surgery.
This webpage explains the key historical clues, symptom patterns, physical examination findings, diagnostic tests, and responses to treatment that help distinguish true intrinsic shoulder pathology (rotator cuff disease, glenohumeral osteoarthritis, acromioclavicular joint arthritis, etc.) from cervical radiculopathy mimicking shoulder pain. The information is based on peer-reviewed orthopedic, neurosurgical, and physical medicine literature.
Very common, and more frequent than one might expect. Studies show that 15–55% of patients presenting with predominant shoulder pain may actually have a primary cervical spine source:
- A 2020 study demonstrated that up to around 50% of patients with shoulder pain being evaluated have some component of cervical disease and radiculopathy contributing to or causing their symptoms(1).
- Patients with severe and treatment resistant tennis or golfer’s elbow commonly have disease sourced from the cervical spine(2).
- A confirmatory test for cervical source of atraumatic shoulder pain is a cervical nerve root block (the gold standard) which can improve the majority of pain symptoms when property done under imaging guidance(3).
Bottom line: If your shoulder MRI is “normal” or only shows mild age-related changes, the neck is a very real possibility.
Symptom Location and Quality – The Dermatome Map Matters
The C5 and C6 nerve roots are the most common culprits for shoulder-area referred pain. The fifth cervical root (C5) causes pain over the lateral shoulder and upper arm (deltoid region). The sixth cervical root (C6) causes pain over the biceps, lateral forearm, thumb, and index finger. However, sometimes the symptoms from cervical radiculopathy do not always have to radiate distally down the arm below the elbow. Sometimes the referred pain from the cervical disease is confined to just the shoulder itself, although other areas such as the armpit or shoulder blade frequently become painful as well (not always).
Patients often say “my shoulder hurts,” but point to the top, back, or outer part of the shoulder — exactly where C5 dermatome pain is felt. In contrast, rotator cuff tendinopathy or tears typically cause pain in the anterolateral arm just below the deltoid, often described as a deep ache worsened by reaching overhead or behind the back.
Experienced shoulder surgeons such as Dr. Thomas Obermeyer and spine specialists use a few quick tests to separate the two. It should be noted no examination test in isolation is perfect and false negatives and false positive tests are not uncommon depending on the pain severity and the individual patient’s response to the disease process.
- Spurling’s Test (foraminal compression test) – While not a great screening test (low sensitivity at around 30-40%), if positive it is very specific(4). If turning and tilting your head toward the painful side reproduces your shoulder or arm pain, this strongly suggests a cervical source.
- Pain with Provocation (Neer/Hawkins) – Positive in true rotator cuff disease, usually negative or inconsistent in pure cervical radiculopathy.
- Rotator Cuff Strength Testing – True weakness (especially external rotation or supraspinatus) points to rotator cuff tear. “Pseudoweakness” from pain inhibition is common in cervical radiculopathy but improves with distraction or cervical traction.
Diagnostic tests, much like physical examination findings, are also imperfect. This is especially the case in older patients which frequently have incidental “wear and tear” type changes that do not always relate to symptoms. As example, patients with shoulder pain from a cervical nerve disorder may have changes in the tendon or labrum of the shoulder reported on MRI but if a scan were to be performed on the other painless side the same changes would be detected.
- Shoulder X-rays & MRI – Excellent for rotator cuff tears/bone spurs, arthritis, calcific tendinitis. Normal or mild findings do not rule out a cervical source.
- Cervical MRI – The single most useful test when history/exam suggests neck origin. Look for foraminal stenosis at C4-5 (C5 root) or C5-6 (C6 root). Disc herniations and spondylotic foraminal narrowing are common.
- Diagnostic Cervical Selective Nerve Root Block – The gold-standard confirmatory test. If injection of local anesthetic around the suspected nerve root (usually C5 or C6) abolishes your shoulder pain for the duration of the anesthetic, the diagnosis is confirmed(1). This is dependent on a qualified proceduralist doing the cervical injection in exactly the right place.
- EMG/Nerve Conduction Studies – Helpful only in advanced cases, especially when weakness or sensory loss is present. Normal in a large portion of cervical sensory (pain only) radiculopathies. In patients with later confirmed cervical nerve disease, it is positive in only 42% of cases(6).
If you have shoulder pain and any of the following, ask your doctor to evaluate your neck.
- Pain started without any injury and gets worse rapidly
- You have neck stiffness or pain with certain head positions
- Pain shoots below the elbow or into the hand
- A subacromial shoulder injection helped only briefly (or not at all)
- Your shoulder MRI is relatively normal for your age
Getting the right diagnosis early can save you months of ineffective physical therapy, unnecessary medications, and even avoidable surgery.
Seek out experienced board-certified fellowship trained shoulder surgeon Dr. Thomas Obermeyer is uniquely qualified to differentiate pain sources and consider a second opinion consultation today to understand your symptoms and ensure surgical decision making is appropriate and needed. Don’t settle for “it’s just arthritis” or “you need rotator cuff surgery” if the story doesn’t add up — a thorough history, targeted physical exam, and selective use of diagnostic tests and procedures can clarify whether your pain is truly coming from the shoulder or is being referred.
References
- Katsuura Y, Bruce J, Taylor S, Gullota L, Kim HJ. Overlapping, Masquerading, and Causative Cervical Spine and Shoulder Pathology: A Systematic Review. Global Spine J. 2020 Apr;10(2):195-208. doi: 10.1177/2192568218822536. Epub 2019 Feb 17. PMID: 32206519; PMCID: PMC7076593.
- Gunn CC, Milbrandt WE. Tennis elbow and the cervical spine. Can Med Assoc J. 1976 May 8;114(9):803-9. PMID: 1268791; PMCID: PMC1957126.
- Takeuchi M, Kamiya M, Wakao N, Osuka K, Yasuda M, Terasawa T, Yamada T, Takayasu M. A simple, 10-minute procedure for transforaminal injection under ultrasonic guidance to effect cervical selective nerve root block. Neurol Med Chir (Tokyo). 2014;54(9):746-51. doi: 10.2176/nmc.oa.2013-0332. Epub 2014 Mar 7. PMID: 24614822; PMCID: PMC4533367.
- Tong HC, Haig AJ, Yamakawa K. The Spurling test and cervical radiculopathy. Spine (Phila Pa 1976). 2002 Jan 15;27(2):156-9. doi: 10.1097/00007632-200201150-00007. PMID: 11805661.
- Rubinstein SM, Pool JJ, van Tulder MW, Riphagen II, de Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007 Mar;16(3):307-19. doi: 10.1007/s00586-006-0225-6. Epub 2006 Sep 30. PMID: 17013656; PMCID: PMC2200707.
- Ashkan K, Johnston P, Moore AJ. A comparison of magnetic resonance imaging and neurophysiological studies in the assessment of cervical radiculopathy. Br J Neurosurg. 2002 Apr;16(2):146-8. doi: 10.1080/02688690220131741. PMID: 12046733.

